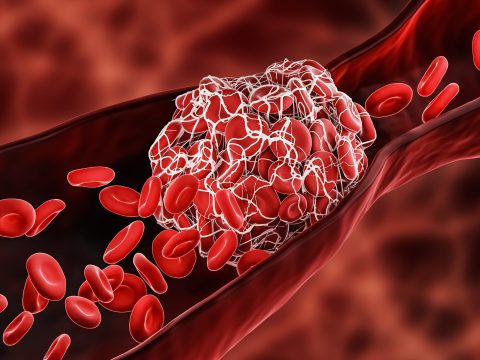
Unfortunately, most people are unaware that they have deep vein thrombosis until they seek emergency treatment for a pulmonary embolism. At Advanced Heart and Vein Center, we are committed to raising awareness of this common medical condition and helping patients understand their risk for blood clots.
Quick Facts About DVT
Here are a few quick facts about DVT/PE in oncology, according to the National Blood Clot Alliance:
- It is estimated that up to 600,000 people in the United States are affected by DVT/PE each year, and that up to 100,000 Americans die each year due to DVT/PE.
- 10% to 30% of people affected by DVT/PE will die within one month of diagnosis.
- In about 25% of people who experience a PE, the first “symptom” is sudden death.
- Among people who have had a DVT, one-third will have long-term complications, such as swelling, pain, discoloration, and scaling in the affected limb.
- One-third (about 33%) of people with DVT/PE will have a recurrence within 10 years.
Symptoms of DVT
DVT causes symptoms in only about half the people who develop this condition. Symptoms may include:
- Swelling of the leg
- Pain or tenderness in the leg
- Increased warmth in the swollen or painful area
- Red or discolored skin in the swollen or painful area of the leg
Some people may not know they have a DVT until it breaks off and travels to the lungs, causing a pulmonary embolism (PE). PE is an emergency situation requiring immediate medical help.
PE symptoms include:
- Sharp chest pain when taking a deep breath
- Shortness of breath
- Bloody cough
- A rapid or irregular heartbeat
- Feeling of anxiety
- Feeling faint or passing out
What Causes DVT?
There are several factors that contribute to the development of DVT, including the following:
- Injuring a vein
- Taking hormones after menopause
- Being immobile
- Chronic health problems, such as heart disease, lung disease, and inflammatory bowel disease
- Having a history of DVT
- Surgery, particularly surgery of the hip or leg
Diagnosing DVT
To determine if DVT is present, your doctor will obtain your medical history and perform an examination. Your diagnostic tests may include:
- Duplex ultrasound: Noninvasive test uses high-frequency sound waves to measure blood flows through your veins and evaluate the presence of clot.
- D-dimer test: Measures a substance in the blood that when elevated may indicate underlying blood clot.
- CT venogram: Imaging test that uses IV contrast and specialized CT scan to create detailed pictures of the veins in your abdomen and legs.
- Venography: Dye is injected into a vein in the affected leg. The dye makes the vein visible on an x-ray image. The x-ray shows whether blood flow is slow in the vein, which may suggest a blood clot.
Complications of DVT
Pulmonary embolism (PE): Most of the time with a DVT, the clot is in the veins of the lower or upper extremities and attached to the vein wall. When the clot dislodges from the vein, it will travel to another part of the body, this is called an embolus. With PE, the clot travels to the lungs and blocks blood flow. As a result, the lungs can be damaged by lack of blood flow, and other organs can be damaged by a lack of oxygen supplied by the lungs. PE is a dangerous, potentially fatal occurrence requiring immediate medical attention.
Post-thrombotic syndrome (PTS): Is a condition that may develop one to two years following an episode of DVT. Following a DVT, the veins involved may be damaged, and there be underlying blockage or reversal of blood flow. Both of these situations can lead to increased venous blood pressure in the legs. The symptoms associated with this condition, known as PTS, may include chronic leg pain and chronic swelling. Advanced stages of the condition include skin damage with discoloration and/or ulceration (wound) in the affected leg.
Treatment Options for DVT
DVTs often can be managed with:
- Blood thinners: The standard of treatment for DVT is blood-thinning drugs such as heparin, warfarin (Coumadin®), or one of the newer oral anticoagulants (Xarelto). A typical course of treatment takes place over three to six months, with periodic blood tests and ultrasounds to evaluate how well the blood thinners are working. In some situations your doctor may recommend lifelong treatment.
- Special compression stockings: Compression stockings may help prevent further clotting, reduce pain and swelling, and prevent the development of post-thrombotic syndrome.
Other treatments include:
Deep vein thrombosis has traditionally been treated with blood thinning medications alone. These medications help prevent early complications such as clot extension and PE. They do not do a good job of preventing PTS. In some situations patients are offered additional treatment to blood thinners. The reason to do this is to prevent damage to the deep veins and prevent developing PTS.
- Thrombolytic therapy: Drugs (clot-busting agents) such as tissue plasminogen activator (tPA) — the same drug used to treat heart attacks — may be used to dissolve and remove clots blocking blood flow through a vein. A small catheter (tube) is placed in the area of the clot which slowly drips tPA directly into the clot to dissolve over several hours.
- Pharmaco-mechanical thrombolysis: Uses specialized devices to deliver “clot-busting agents” and mechanically break down the clot. This may be used in situations with extensive clot in the leg and allows less usage of tPA and quicker removal of clot.
- Inferior Vena Cava Filter
- Clot Removal
Preventing DVT
Recognizing individual risk and providing appropriate prophylaxis is important. There are steps that can be taken to prevent DVT and pulmonary embolism during hospitalization or travel.
When hospitalized:
- Know what your risk is for developing a DVT. Take a risk assessment.
- Talk to your doctor about your risk of DVT and what can be done to help protect you.
- Get out of bed as soon as possible as your doctor recommends. Walking reduces the chance of developing a blood clot.
- Take medicines (low-dose blood thinners) that your doctor prescribes to prevent blood clots.
- Use compression boots while in bed as your doctor directs. These boots squeeze your legs to promote blood flow in the veins and help prevent DVT.
When traveling:
- Know your risk of DVT. Schedule a risk assessment at our clinic.
- Walk up and down the aisles of the plane, bus or train. If traveling by car, stop about every hour and walk around.
- Flex, stretch and move your legs and your feet to improve blood flow in your calves.
- Wear loose and comfortable clothing.
- Drink plenty of fluids and avoid alcohol.
- If you have risk factors for DVT, your doctor may advise you to wear compression stockings while traveling.
- If you have had DVT or pulmonary embolism previously, you may be prescribed a blood-thinning medicine before traveling.